Improved post-diagnostic information and support is recognised in Scotland’s National Dementia Strategy as one of two key service delivery areas in which immediate change is required. There is clear evidence that high quality post diagnostic support, provided over an extended period, is essential in order to equip people with dementia and their families and carers with the tools, connections, resources and plans they need to live as well as possible with dementia and prepare for the future. The positive effect which this kind of support can have on people’s lives has been demonstrated in the post diagnostic support pilot funded by the Scottish Government and delivered by Alzheimer Scotland, and international evidence shows the long term impact in reducing and delaying the need for care services.
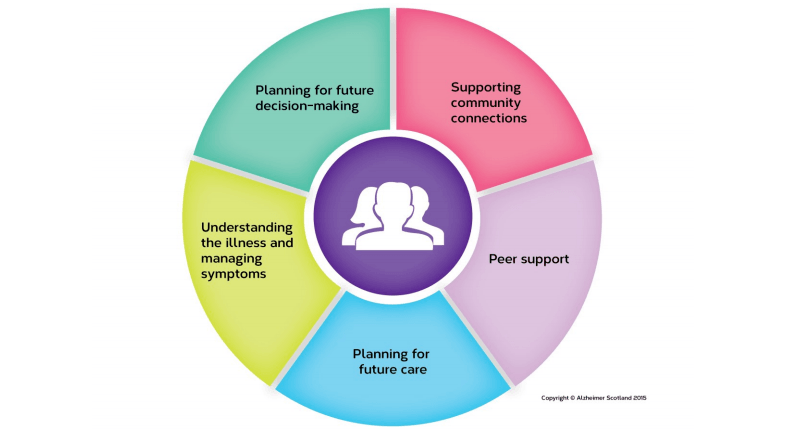
There are five key pillars which are recognised as essential to supporting people after their diagnosis, outlined in the diagram above.
The purpose of the guarantee is to provide the security, for a minimum of one year, of a named person who has the flexibility to work alongside the person, their partner and family and ensure that over that 12 month period each person is given help and support to work through the five pillars. By the end of the year it is expected that some individuals might require ongoing professional support; however the purpose of the post diagnostic support is to enable the individual and their family to develop a robust personal plan that utilises all their own natural supports, that maintains newly developed peer support mechanisms alongside existing and new community connections and that will support each person to live well and independently with dementia for as long as possible.
It is imperative that post diagnostic support is personalised and flexible, and delivered proactively and sensitively over the course of a year by a skilled and well-trained person, who can develop a supportive relationship with the individual and their partner and family.
There is no preferred systematic order in delivering this support; each person will need a unique approach and professionals will need to identify when that person and their family are ready to engage in each area. Some people will need time without too much support to absorb a diagnosis of dementia; others might need to begin planning their future right away, while others might need help to maintain their community connections and not withdraw from aspects of everyday life that are keeping them active and engaged.
The five pillars highlight key areas of activity. Various techniques and approaches can be used to deliver a given pillar, but it essential that the full range is offered to each person. Some examples of what this will mean in practice and suggested techniques are outlined below:
1. Help to understand the illness and manage its symptoms – supporting people with dementia and their partners and families to come to terms with dementia and learn to self-manage their condition. This pillar must involve the person’s family and natural support network. It will mean breaking away from the traditional patient-professional model, to a more patientfamily/network model of living with dementia. Approaches such as Family Group Conferencing and other methods of family engagement will inform this work.
2. Support to stay connected to their community – working closely with people to maintain and build on their existing social networks, to enhance their quality of life and maximise the natural support they receive from those around them, helping to avoiding isolation and reducing future reliance on care services. This will require a shift away from traditional health and social care boundaries. The named worker will need to work with the person to enable risk, plan purposeful community activity and connection, and to engage with community development partners and organisations to help people with dementia continue to use and be fully included in mainstream community activity.
3. Peer support from other people with dementia and their families and carers – this is highly effective in helping people come to terms with the illness and find coping strategies, and in maintaining their wellbeing and resilience. A good example of peer support is the dementia cafés run by Alzheimer Scotland and others. These allow people with dementia and their families and carers to attend together, in a relaxed informal atmosphere where they can get information from professionals but, most importantly, have the opportunity to meet other people facing similar challenges. Feedback from people using the cafés in Alzheimer Scotland’s post-diagnostic pilot shows how much they value this. They said that the cafés helped in all kinds of ways, helping them see how you can live positively with dementia and helping families to think about balancing independence with risk. Having a forum for open discussion of these issues helped everyone to cope better, and enabled greater independence and reduced frustration all round.
4. Help to plan for their future decision-making – support to set up powers of attorney and other statements of their wishes while they are able to make their own choices about the future. This will include dealing with very sensitive issues in a skilled and informed manner. It also gives a focus to issues such as advance directives and Adults with Incapacity issues and will also ensure that each person has a good understanding of Self Directed Support.
5. Support to plan the shape of their future care from their own perspective – together with those around them, developing a personal plan with their choices, hopes and aspirations, which can guide professionals. Person-centred planning offers a variety of tools and techniques to assist this process. This approach has been used extensively in other fields of practice, but not previously with people with dementia.
The Alzheimer Scotland pilot showed that existing tools can be successful adapted to help people with dementia to think creatively about the support they might require and about how the people around them can offer support. The basis of person-centred planning is that the emphasis shifts away from professional inputs and expectations. Instead, it builds on the hopes and expectations of the person and their family and uses techniques to place these hopes and personal outcomes at the centre of practice.
It goes beyond person-centred approaches and converts the person’s hopes into a live plan, with a series of goals, steps and outcomes that those involved in that person’s life will help to deliver. In this scenario, professionals are equal contributors alongside family and friends and the focus is always on the person. The person owns the plan and it can be used to lead future interventions and as a method of planning transitions.
Other methods exist to develop and work towards a more personal outcomes-based approach, such as the use of Talking Points. The named person should be equipped to use and have access to a range of interventions and planning tools that he/she can offer to each person. The essential focus must be on supporting personal choice, personal strengths and achieving individual outcomes. How this is achieved will be varied and highly personalised.